5 Symptoms of Depression You Shouldn't Ignore
5 Symptoms of Depression You Shouldn't Ignore
Feeling sad after a difficult day is normal. Feeling down for a few days after a loss or disappointment is part of being human. But when does sadness cross the line into something more serious? Depression is a mood disorder that causes feelings of sadness that won't go away—and understanding the difference could be the first step toward getting help.
Whether you're in Baltimore, Towson, Columbia, or elsewhere in Maryland, recognizing the symptoms of depression is important. Depression is not a weakness or a character flaw. It's a common medical condition—and it's treatable.
What Exactly Does Depression Do?
Depression is a mental state that negatively affects how you feel, think, act, and perceive the world. It's more than just feeling sad. Depression, also called major depressive disorder or clinical depression, is one of the most common mental disorders.
Depression can cause sadness, loss of interest in activities, changes in sleep or appetite, trouble concentrating, and low energy. Some people may also feel hopeless or have thoughts of self-harm. Depression affects people of all ages, races, biological sexes, income levels, and educational backgrounds.
How Common Is Depression?
Approximately one in six people will experience a major depressive episode at some point in their lifetime. Depression often begins in the teens, 20s or 30s, but it can happen at any age. More women than men are diagnosed with depression, and younger adults are more likely than older adults to experience depression.
What Causes Depression?
There is no single cause of depression. Depression can happen to people of any age, background, or gender. Research suggests it's caused by a combination of biological, social, and psychological factors:
Brain chemistry - Disruptions in neurotransmitters like serotonin may play a significant role
Family history - A history of mental disorders in close relatives increases risk
Life events - Adverse life events, such as bereavement and trauma, can contribute to developing depression. Individuals who experienced four or more adverse childhood experiences are 3.2 to 4.0 times more likely to suffer from depression
Stressful circumstances - Stressful life events, unemployment, or financial difficulties increase depression risk
Medical conditions - Chronic pain and some medical conditions can increase risk
Psychological factors - Negative thought patterns and coping behaviors increase vulnerability. Low extraversion and high neuroticism are associated with higher depression risk
For adolescents, depression may develop following social rejection, peer pressure, or bullying. Living in large urban areas is linked to lower rates of depression compared to smaller towns and rural areas.
Depression vs. Normal Sadness
It is normal to experience moments of sadness as part of the human experience. Everyone feels down sometimes. The key difference is duration and impact: a diagnosis of depression requires symptoms to persist for at least two weeks and cause noticeable problems in daily activities.
With normal sadness, you can usually still function—go to work, maintain relationships, and find moments of enjoyment. With depression, everyday activities become extremely difficult or impossible. Depression often causes noticeable problems in day-to-day activities, such as work, school, social activities or relationships with others. Living with depression can lead to emotional, behavioral, and health problems that affect every area of life.
What Are 5 Symptoms of Depression?
According to the Diagnostic and Statistical Manual of Mental Disorders published by the American Psychiatric Association, symptoms of depression can vary from mild to severe and may appear differently in each person. Here are five key symptoms that shouldn't be ignored:
We often tell clients in our Baltimore practice that recognizing depression symptoms is the first step many people take toward feeling better. One of the biggest challenges we see is people dismissing their own suffering because they think they should be able to "just push through it." Depression isn't laziness or weakness—it's a medical condition with real biological underpinnings. When clients finally understand this, they stop blaming themselves and start focusing on treatment that actually works.
1. Persistent Sadness or Depressed Mood
The persistent feelings of sadness caused by depression can result in withdrawing from activities and responsibilities. This isn't just feeling blue for a day or two. We're talking about a depressed mood that lasts most of the day, nearly every day, for at least two weeks.
People with depression may feel generally miserable or unhappy without fully understanding why. The sadness feels overwhelming and inescapable. Some people describe it as feeling empty, numb, or hopeless rather than actively "sad." This persistent sadness doesn't lift even when circumstances improve.
2. Loss of Interest or Pleasure in Activities
Losing interest in things you used to enjoy is one of the hallmark symptoms of depression. This symptom, called anhedonia, means you no longer find pleasure in hobbies, social activities, or things that once made you happy.
You might stop seeing friends, skip activities you previously looked forward to, or lose interest in hobbies. Sex may no longer feel pleasurable. Food might lose its appeal. Even activities you know should make you happy just feel flat and meaningless.
This loss of interest often leads to isolation, which can make depression worse, creating a cycle that's hard to break.
In our years working with depression, we've noticed a pattern: people start canceling plans, then stop making plans altogether, then wonder why they feel so disconnected and alone. The isolation feels protective in the moment—you're too exhausted or sad to socialize—but it actually feeds the depression. We work with clients in Towson and Baltimore to gradually rebuild connections, even when it feels impossible. Social withdrawal is both a symptom and a maintaining factor of depression, which is why addressing it is crucial for recovery.
3. Changes in Sleep, Appetite, or Energy
Depression causes significant physical symptoms that affect your body, not just your mind. These changes include:
Sleep disturbances:
Insomnia (trouble falling asleep or staying asleep)
Sleeping too much (hypersomnia)
Waking up very early and being unable to go back to sleep
Sleep that doesn't feel refreshing, no matter how long you sleep
Appetite and weight changes:
Significant weight loss when not dieting
Significant weight gain
Eating much less than usual or losing your appetite
Eating much more than usual, often seeking comfort in food
Energy problems:
Persistent fatigue and low energy, even after rest
Feeling physically slowed down
Simple tasks requiring enormous effort
Exhaustion that doesn't improve with sleep
These physical symptoms aren't just side effects of feeling sad—they're core symptoms of depression. Medical conditions and some medications can also increase risk of depression, which is why it's important to see a healthcare provider for proper diagnosis.
4. Difficulty with Thinking, Memory, and Concentration
Individuals with depression may experience difficulty with thinking, memory, eating, and sleeping. The cognitive symptoms can significantly impact work, school, and daily functioning.
You might notice:
Trouble concentrating on tasks or conversations
Difficulty making decisions, even simple ones
Problems with memory—forgetting appointments or conversations
Slowed thinking or feeling mentally "foggy"
Trouble focusing enough to read, watch TV, or follow conversations
These cognitive changes can be frustrating because they affect your ability to work and manage daily responsibilities. Some people worry they're developing dementia, when actually these symptoms are part of depression.
5. Feelings of Worthlessness, Hopelessness, or Thoughts of Self-Harm
Depression often brings intense negative thoughts about yourself and the future. Depression can lead to feelings of hopelessness and helplessness, which can impact one's motivation to seek help.
Warning signs include:
Feelings of worthlessness or excessive guilt
Believing you're a burden to others
Feeling hopeless about the future
Thoughts that life isn't worth living
Thoughts of death or suicide
Making plans for suicide
Some people may also feel hopeless or have thoughts of self-harm. If you're having thoughts of suicide, this is a medical emergency. Call 988 for the Suicide & Crisis Lifeline, which offers free, confidential support and emergency counseling 24/7. You can also contact Baltimore Crisis Response, Inc. (BCRI), which provides 24/7 community-based behavioral health crisis response services.
We approach thoughts of self-harm with immediate seriousness and without judgment. In our practice, we've learned that many people hesitate to mention suicidal thoughts because they fear being hospitalized or labeled. The truth is that most people with these thoughts can be treated safely as outpatients. What matters most is that you tell someone—a therapist, doctor, or trusted person. These thoughts are a symptom of depression, and like other symptoms, they respond to treatment. You don't have to face them alone.
Other Symptoms of Depression
Beyond these five key symptoms, depression can cause other symptoms that vary from person to person:
Irritability or restlessness
Physical aches and pains with no clear medical cause
Crying spells
Anxiety or feelings of panic
Moving or speaking more slowly than usual
Avoiding social situations and activities
Depression can manifest differently in children and teenagers compared to adults. In young people, depression might look like irritability, anger, or behavioral problems rather than obvious sadness. Older adults may experience different or less obvious symptoms of depression, which often leads to misdiagnosis. In older populations, physical symptoms or memory concerns may overshadow mood symptoms.
Types of Depression and Depressive Disorders
Depression isn't a one-size-fits-all condition. The term "depression" actually encompasses several types of depressive disorders:
Major Depressive Disorder (Clinical Depression)
Major depressive disorder is the most severe type of depression, also called clinical depression. It involves experiencing five or more depression symptoms nearly every day for at least two weeks, with at least one symptom being either persistent sadness or loss of interest in activities.
Persistent Depressive Disorder
Persistent depressive disorder involves a chronic form of depression lasting for at least two years. Symptoms may be less severe than major depression but are longer-lasting. This condition was previously called dysthymic disorder or dysthymia.
Seasonal Affective Disorder
Seasonal affective disorder is a specific form of depression that occurs seasonally, typically during fall and winter when there's less natural sunlight. Symptoms begin during specific seasons and lift when the season changes.
Perinatal Depression
Perinatal depression, previously known as postpartum depression, can occur during pregnancy or after childbirth. This is more than the "baby blues"—it's a serious depressive disorder that requires treatment.
Bipolar Disorder (Manic Depression)
Bipolar disorder includes episodes of depression alongside episodes of mania or hypomania. Previously called manic depression, this mood disorder involves cycling between depressive episodes and periods of abnormally elevated mood and energy. Bipolar disorder requires different treatment than unipolar depression.
Other Mood Disorders
Other depressive disorders include:
Premenstrual dysphoric disorder - A severe form of premenstrual syndrome that includes significant depressive symptoms
Disruptive mood dysregulation disorder - Characterized by recurrent temper outbursts and an irritable mood in children and adolescents
Understanding which type of depression you have helps guide proper diagnosis and treatment planning.
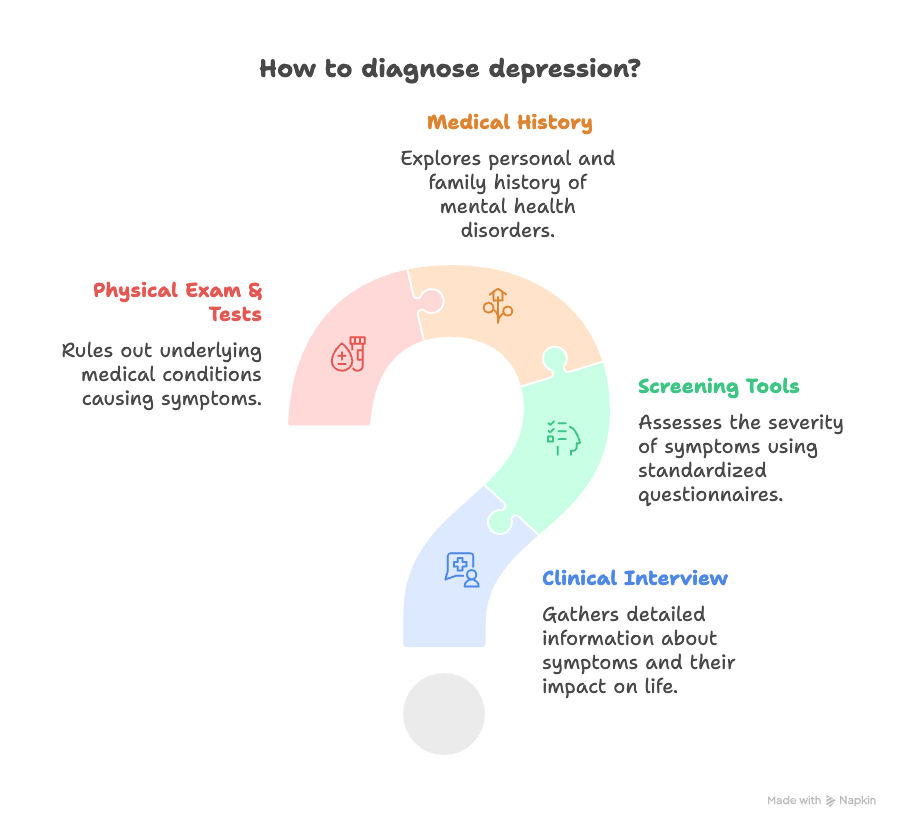
How Is Depression Diagnosed?
Doctors use questions and screening tools, like the PHQ-9, to check for depression. Trained health care providers may ask about your mood, sleep, appetite, energy, and thoughts. The diagnostic process typically includes:
Clinical interview - Your healthcare provider will ask about your symptoms, how long you've had them, and how they affect your life
Screening tools - Standardized questionnaires that help assess the severity of depression symptoms
Medical history - Questions about your personal and family history of mental health disorders
Physical exam and medical tests - To rule out underlying medical conditions that could cause depressive symptoms
Sometimes, depression can be linked to other health conditions. Medical conditions and some medications can increase risk of depression, so your doctor may ask about your medical history and any medicines you take. For some individuals, depression may be a symptom of another underlying condition or disorder, such as thyroid problems, vitamin deficiencies, or other medical issues.
A proper diagnosis is essential because different types of depression and other mental disorders may require different treatment approaches.
What to Do If You're Really Depressed
If you recognize these symptoms in yourself or someone you love, know that help is available. Depression is treatable. Here's what to do:
Immediate Steps
Reach out to someone - Talk to a friend, family member, or trusted person about how you're feeling
Contact a healthcare provider - Make an appointment with your doctor or a mental health professional
Use crisis resources if needed - If you're having thoughts of self-harm, call 988 (Suicide & Crisis Lifeline) or contact Baltimore Crisis Response, Inc. (BCRI)
Treatment Options
The best treatment depends on how severe your symptoms are, your preferences, and what has worked for you before. It is recommended to work with a doctor or mental health professional to develop a personalized treatment plan for depression.
Psychotherapy (Talk Therapy): Many people benefit from talking with a therapist. Cognitive behavioral therapy (CBT) is effective in treating depression by teaching skills to better manage negative thoughts. In addition to CBT, other proven psychological treatments include behavioral activation, mindfulness, and psychodynamic psychotherapy. Psychotherapy may last a few weeks, a few months, or longer depending on the severity of the depression. Talk therapy can be done individually or in group treatment settings.
Medication: Medications such as antidepressants can be helpful in alleviating depressive symptoms. Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed antidepressant medications. Antidepressants may produce some improvement within the first week or two of use, but full benefits may not be seen for two to three months. Your healthcare provider can help determine if antidepressant medication is right for you.
Lifestyle Changes: For mild depression, lifestyle changes that improve sleep habits, exercise, and address underlying health conditions can be an important first step in treating depression. Regular exercise helps create positive feelings and improves mood for many people experiencing depression. Other helpful lifestyle adjustments include maintaining a healthy diet, establishing good sleep habits, and staying connected with others.
Finding Help in Baltimore
Numerous resources are available in Baltimore for individuals struggling with depression:
Baltimore Therapy Group - Schedule an appointment with experienced therapists in Baltimore, Towson, or Columbia
Baltimore Crisis Response, Inc. (BCRI) - 24/7 community-based behavioral health crisis response services
The National Alliance on Mental Illness (NAMI) Metropolitan Baltimore - Offers support groups and educational resources
The Pro Bono Counseling Project - Connects uninsured or underinsured Maryland residents with volunteer mental health professionals
Online directories - Psychology Today or WithTherapy.com can be used to find therapists and psychiatrists in the Baltimore area
Stigma surrounding depression may prevent people from seeking help, making their daily struggles more difficult. Remember: seeking help is a sign of strength, not weakness.
5 Coping Skills for Depression
While professional treatment is important for moderate to severe depression, these coping skills can help manage symptoms and support your recovery:
1. Stay Active with Behavioral Activation
When you're depressed, you naturally want to withdraw and isolate. Behavioral activation—deliberately engaging in activities even when you don't feel like it—is one of the most effective coping behaviors for depression. Start small: take a short walk, call a friend, or do one small task. Schedule enjoyable activities and breaking problems into smaller steps can also make a difference.
2. Exercise Regularly
Regular exercise helps create positive feelings and improves mood for many people experiencing depression. You don't need to run marathons—even 20-30 minutes of walking can help. Exercise affects brain chemistry in ways that can reduce depressive symptoms.
3. Maintain Sleep Hygiene
Since sleep problems are both a symptom and a contributor to depression, improving sleep habits is crucial. Go to bed and wake up at the same time daily, avoid screens before bed, and create a relaxing bedtime routine.
4. Stay Connected
Depression makes you want to isolate, but social connection is vital for recovery. Reach out to friends and family, even when it feels hard. Lifestyle adjustments and social support are crucial for overall management of depression.
5. Practice Self-Compassion
Depression often comes with harsh self-criticism. Practice talking to yourself the way you'd talk to a good friend going through a hard time. Remind yourself that depression is a medical condition, not a personal failing.
These coping skills work best alongside professional treatment, not as a replacement for it. If you're experiencing severe symptoms, thoughts of self-harm, or symptoms that interfere with daily functioning, professional help is essential.
The Bottom Line
Depression is not a weakness or something you can just "snap out of." It's a real medical condition that affects millions of people—and it's treatable. If you're experiencing persistent sadness, loss of interest, changes in sleep or appetite, difficulty concentrating, or feelings of hopelessness for more than two weeks, reach out for help.
Living with depression can lead to emotional, behavioral, and health problems that affect every area of life. Depression can significantly reduce the quality of life for both the individual and their family. But with proper diagnosis and treatment—whether that's psychotherapy, medication, or a combination—most people with depression see significant improvement.
You don't have to struggle alone. Help is available in Baltimore and throughout Maryland.
Disclaimer: This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified mental health provider with any questions you may have regarding a medical or mental health condition. If you are in crisis or experiencing thoughts of self-harm, please call 988 (Suicide and Crisis Lifeline) or go to your nearest emergency room.